
Pregnancy and iron deficiency
It costs 1000 mg of iron to make a baby. It’s a loss unless we replenish it. So we should do that.
In the First Trimester
There is a prevalence of around 12% at the beginning of pregnancy, which increased during pregnancy up to 65%. Some studies have revealed rates up to 80% iron deficiency rates in pregnancy.
The iron requirement in the first trimester is 1-2 mg per day. That’s one burger every day.
*PS my apologies to the vegetarians/vegans for using hamburgers as the marker for iron consumption.
We assume, incorrectly, that women are able to intake and absorb enough iron to make up for this requirement and save up enough for the eventual needs of the rest of the pregnancy and delivery.
Some roadblocks to this are:
Nausea and vomiting of pregnancy.
Inability to take a prenatal vitamin.
Oral iron causing nausea and constipation.
All, which set you up to have even greater issues later on in pregnancy because the vault is empty.
Now this all assumes there’s no other reason ie: colitis, celiac, vegetarianism that could add to the iron loss during an otherwise normal pregnancy.
Prenatal supplements contain iron at various forms and dosages.
In the Second Trimester iron deficiency
4-5 mg of loss per day because of placental growth. Imagine this is another 2 burgers.
Third Trimester iron deficiency
7.0 mg of loss per day by due date. You’ve lost another 3 burgers per day.
If you’re 30 weeks pregnant and have low iron (ferritin <30) you should get an iron infusion.
Why?
While anemia is roughly a hemoglobin less than 110 g/L (11 g/dL), iron deficiency is currently a ferritin score of 30 or below.
Guidelines for iron infusions in pregnancy are clear that there are many scenarios you not only qualify for, but should get an infusion.
You should qualify for an infusion instead of taking oral iron if:
Your hemoglobin in the 3rd tri is <100 g/L (10 g/dL)
You have a hard time taking oral iron, whether it bothers you or you don’t remember to take it.
You have a condition that prevents you from absorbing oral iron.
Oral iron just isn’t working.
There’s one more reason that’s rarely encouraged.
30 weeks of pregnancy with ferritin <30. It’s as simple as that.
Why should you get an iron infusion while pregnant?
By this milestone, it’s virtually impossible to get your iron levels up to where they need to be by the time you deliver your baby, no matter how you deliver your baby. Iron infusions easily solve this problem.
Let’s say you don’t fall into these criteria and you want an infusion, they aren’t set in stone. You and your healthcare provider can decide based on your preferences whether iron infusions are right for you.
We don’t need pregnancy to be complicated by simple preventable measures. If your healthcare provider isn’t up to date with these guidelines, advocate for yourself. Use this site as a reference tool to do so.
1 in 3 pregnant women have not had their iron levels checked by the time of giving birth. In women who were identified as being deficient, less than half were treated with iron. ref
You might be fine going into pregnancy because 12% of women are iron deficient at the beginning of pregnancy. That number soars to 65% by the end of pregnancy. ref
Women who give birth while iron deficient risk their babies suffering consequences that matter. Iron deficiency is a risk factor for preterm delivery, low birth weight and infant health post delivery, well into adulthood.
It’s optimal to address iron deficiency before the third trimester of pregnancy. Neurogenesis, which relies on iron, peaks during the third trimester and early neonatal stages. Iron deficiency is linked to impaired neurocognitive development in children.
PostPartum iron deficiency
If somehow you’ve been able to get past the iron gauntlet of pregnancy and be one of the minority who come out with normal iron scores, you now have to deal with the loss of blood from delivery.
Vaginal Delivery = 250 mg of iron loss
C Section = 500 mg of iron loss
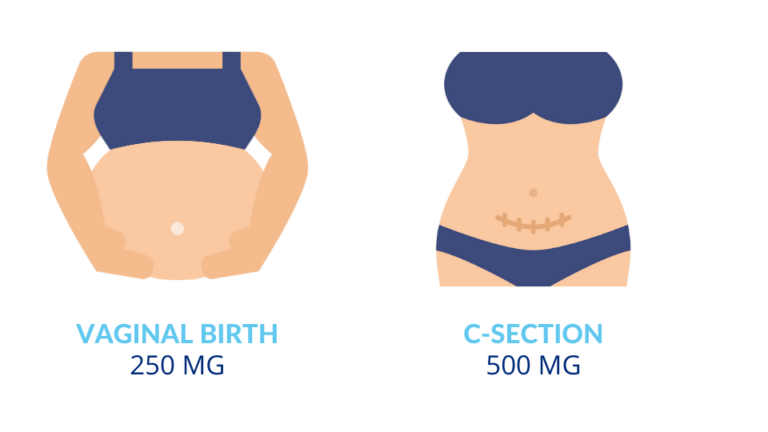
If you’re iron deficient post-partum it can be challenging for your energy and mental health.
No matter what stage of pregnancy, knowing your iron status is paramount. If you’re deficient, it could have far reaching consequences for mother and baby. We don’t test and treat enough. We need to correct this deficiency now.
References:
J Nutr. 2022;152(10):2238.
J Matern Fetal Neonatal Med. 2021;34(6):1002. Epub 2019 Jun 3.
Blood Adv. 2021;5(22):4666.
Food Sci Nutr. 2021 Dec; 9(12): 6559–6565.
Front Hum Neurosci. 2013; Sept 23(7): 585.





